I just looked at the map again to make sure I know where the parking garage is.
I’ve been to Vanderbilt many times at this point to see my pulmonologist, but I always double check the map before an appointment.
Tomorrow is my next appointment with her. I currently see her every 6 months to monitor the status of my pulmonary arterial hypertension (PAH).
I usually have an appointment over the summer, but with my big road trip, I had to push it out a few months.
Ironically, November is Pulmonary Hypertension Awareness month, so it seems fitting.
I’ve grown accustomed to these appointments since being diagnosed with my conditions in 2021. I’ve always had about an hour drive to see my pulmonologist. Previously, I saw a specialist at the UC Health Hospital in Aurora, CO.
Drive an hour there. Park in the garage. Walk to the clinic. Find the bathroom. Check in. Wait.
Waiting rooms used to scare me, but now they are just a place to pause before what comes next.
After waiting for a bit, they take me back to get my weight and check my vitals. The nurse will leave. I’ll wait a few more minutes, then someone will come get me to take me to do my 6-minute walk.
The 6-minute walk test is used to gauge the status of my overall condition, as well as how efficiently my medications are working.
There are 4 types of medications for PAH including tablets which are swallowed, some which are inhaled, ones that are injected, and some that require an IV.
When I was first diagnosed 4 years ago, I was told I would need the most drastic measures, because of the severity of my PAH. This includes intravenous therapies and subcutaneous therapies.
I was told that I would HAVE to go on IV medication at some point and I would be wearing a pump strapped to me at all times for the rest of my life.
I said no.
I told the doctors I only wanted oral medications.
I was put on a combination of oral therapies and re-tested 6 months after my original diagnosis. The results from the right-heart cath showed no improvement, and in fact, showed slightly higher numbers.
They told me I wasn’t doing enough, I needed more meds. Stronger meds.
I said no.
Instead, I asked if moving to a lower elevation would help?
They said no.
I metaphorically told them to hold my beer and booked a trip to Tennessee.
On that trip, I felt stronger than I had in more than a decade and I even managed to walk 13k steps at Dollywood – something that I hadn’t accomplished in a very long time. It was then that I knew part of the way I was going to manage this condition was by moving to a lower elevation.
…
Diagnosis and prognosis.
Doctors think that within those 2 terms, a patient’s life is black and white.
You have a disease.
Here are some meds to manage it.
You will live roughly this long and only be able to do x, y, and z.
Again, I’m not a sith, so I don’t deal in absolutes.
I’m not saying doctors don’t care, but their education is not holistic, so why would their care plan be?
I had a couple doctors look me in the eye in Colorado and tell me, definitively, my quality of life would never improve and there were certain things I would never do again. Again, hold my beer.
I accepted my diagnosis – it made sense. I had been struggling for years with edema, shortness of breath, dizziness, lack of energy, and several other symptoms that align completely with PAH. While shocking to actually receive, the diagnosis was actually a helpful confirmation so I could put a name on what I was up against.
The prognosis is where they lost me.
When the term PAH was first thrown out there by my cardiologist, I spent an entire night Googling what I thought was my death sentence.
Things kept coming up like:
- Rare
- Progressive
- Right-sided heart failure
- Poor quality of life
- Cause unknown
- No cure
- Limited exercise capacity
- Women with PAH should not have children
- And so on…
I couldn’t accept any of that, so I simply didn’t.
I started figuring out my own prognosis, because there was no way any human being on this earth, or Google, was going to tell me how the rest of my life was going to work out.
For the last 4 years, I have worked tirelessly to write my own prognosis.
- It started with the move to Tennessee – I had to get to a lower elevation as quickly as possible so I could get a grip on things.
- I found a supportive pulmonologist at Vanderbilt who was willing to listen to me and be part of MY plan for my care. She understands and encourages my holistic methods that pair alongside the medications I currently take (which are the same ones I had at diagnosis by the way. I have never added stronger ones).
- I started eating clean.
- I started moving regularly.
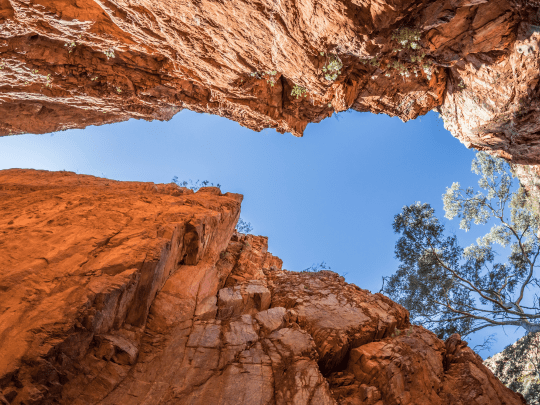
- I started spending time in nature.
- I removed toxic behaviors, and those who engage in them, from my life.
- I started strength training.
- I started getting rid of all my stuff.
- I became a teacher.
- I accepted that my dreams may turn out differently than planned, but they are still completely possible.
- I stopped worrying about being part of the 61% and just kept going.
Doctors gave me a diagnosis and for that I am grateful.
God is going to help me shape the prognosis though, and that, no one can change.
If this disease was supposed to kill me it would have already done it when I was sleeping for years, hypoxic, with my oxygen dipping into the 60s.
This disease doesn’t define me, and it certainly will not get credit for my cause of death, when I’m still alive and fighting.
The diagnosis was a starting point, but my prognosis has been a beautiful exploration of what can actually be done when you have faith, hustle, and trust that the body can in fact heal.
I’m not sure exactly how far I’ll walk on my 6-minute walk tomorrow or what my bloodwork numbers will be, but I can move with confidence that each appointment from here on out will show that I never gave up and will never surrender to my original “prognosis.”
❤






Leave a comment